Advancements and Challenges in Breast Cancer Diagnostics
In breast cancer diagnostics, early and accurate detection remains paramount. Despite technological advances, significant challenges continue to shape the practice, from patient comfort to the effectiveness of imaging in different breast densities. Guido Gebhardt spoke with Dr. Wasser, an experienced radiologist in breast imaging at the Leiden University Medical Centre LUMC Department of Radiology, about the intricacies of screening methods and new modalities that could revolutionize the early detection of breast cancer.
What are the Challenges in Breast Cancer Diagnosis?
Early detection is a fundamental challenge in diagnosing breast cancer, highlighting the importance of regular screening. Detecting cancer at its earliest possible stage is crucial. However, many women are reluctant to undergo mammography due to discomfort from breast compression during the procedure. This discomfort discourages participation in population screening programs.
Mammography, the current standard screening technique, also faces technical limitations, particularly in women with dense breast tissue. In such cases, mammography may miss cancerous tissues, leading to “interval cancers”— cases where a tumor is visible only a few years after a negative mammogram, suggesting it might have been undetectable due to overlapping normal breast tissue. The key challenges are enhancing screening participation and optimizing the technology to detect cancers as early as possible.
Which Imaging Modalities are Used in Routine Diagnostics and Mammo Screening?
In clinical practice, mammography and MRI serve as primary tools for breast imaging. Mammography is typically the first-line method for screening. If an anomaly appears on the mammogram, we usually follow up with an ultrasound, which allows for a biopsy in the same session if necessary. In cases where a patient is at high risk for breast cancer, MRI is often used either as a primary or supplementary modality.
MRI is highly sensitive for detecting both invasive cancer and pre-malignant conditions such as ductal carcinoma in situ (DCIS). However, limitations exist for mammography, especially in patients with dense breasts, where additional methods are required to ensure accuracy.
Could Breast CT be a Promising Addition to the Diagnostic Toolbox?
In recent years, breast CT has emerged as an alternative screening tool. We introduced at LUMC approximately three years ago, AB-CT’s nu:view breast CT. The scanner offers several advantages over traditional mammography, tomosynthesis, and MRI. One significant benefit is its appeal to women who previously avoided screening due to discomfort from compression in mammography. Since breast CT does not require compression, many women who previously declined screening are now participating, making it possible to detect larger tumors or multifocal cancers that may have otherwise gone undiagnosed.
Breast CT allows for a pain-free experience, thus expanding the screening pool. Following an initial awareness campaign, the word spread among patients who actively encourage others to try the procedure.
Comparative Merits of Mammography, MRI, and Breast CT
AB-CT’s nu:view breast CT combines the advantages of both mammography and MRI. Mammography provides a broad overview with simple oblique and craniocaudal (CC) images, making it straightforward for radiologists to review. However, mammography’s two-dimensional nature and limited capability to identify tumors in dense breast tissue can restrict its effectiveness. MRI, on the other hand, offers detailed, three-dimensional imaging with high sensitivity, especially after administering contrast, which highlights malignant tumors. The drawback is that MRI does not display calcifications, which mammography does well.
Breast CT incorporates these strengths: it offers 3D imaging similar to MRI, captures high-resolution images that display tumor morphology more clearly and can show calcifications, which are vital markers for breast cancer. When used with contrast, breast CT can display enhancing tumors like MRI, making it a compelling alternative.
Tomosynthesis, or 3D mammography, is a pseudo-3D technology with a limited tomo-angulation. In patients with dense breasts, it may still miss tumors due to overlapping tissue, whereas breast CT provides true 3D imaging that minimizes these limitations.
Are there already Scientific Studies Showing an Emerging Evidence?
Although breast CT shows promise, comprehensive, comparative studies are still needed to establish its efficacy. Few studies currently compare breast CT directly with mammography or MRI. To validate the clinical role of breast CT, rigorous multicenter studies are essential.
One recent study, published in July from Erlangen, compared breast CT with mammography without contrast. Breast CT with contrast generally outperforms mammography across all breast density categories. Without contrast, however, its performance in dense breasts remains less favorable compared to mammography.
Additionally, advancements in contrast-enhanced mammography (CEM) indicate potential improvements in diagnostic accuracy. Like breast CT, CEM highlights enhancing tumors, but it remains a 2D technique. Its efficacy relative to breast CT, which offers both 3D imaging and higher patient comfort, is still under study. At LUMC, we're performing a multicenter study comparing breast CT with MRI.
What is Your Vision of the Future of Diagnostic Workflow and Population Screening?
In the future, I expect a more efficient workflow where breast CT could gradually replace mammography in diagnostic settings. However, it may face challenges in widespread screening due to the need for contrast. Breast CT is likely to become a primary modality for diagnostic work if it proves at least as effective as mammography. For routine population screening, however, mammography will likely remain the first-line choice in the near future due to its cost-effectiveness.
Ultimately, an ideal workflow would involve mammography for initial screenings, followed by breast CT as a diagnostic tool for patients with inconclusive results or dense breast tissue. This approach could optimize the balance between accuracy, efficiency, and patient comfort.
We Talked a lot about Technology now. Do Patients See or even Feel the Difference a Breast-CT makes?
In a study, we showed that patients overwhelmingly prefer breast CT over mammography, primarily due to the absence of compression. Patients dislike the discomfort of mammography, and breast CT addresses this issue effectively. In our comparison study between MRI and breast CT, preliminary results reveal that most women favor breast CT, citing the shorter duration and lower anxiety levels compared to MRI.
Despite its sensitivity, MRI can induce claustrophobia and discomfort due to the lengthy examination time and enclosed space. With breast CT, patients are finished in about three minutes and do not need to lie in a tunnel, which is a significant improvement over MRI for many.
What are the most important Advantages of Breast CT Technology?
Breast CT’s high-resolution images and comprehensive visualization capabilities make it a valuable diagnostic tool. The resolution of breast CT is excellent; the images are crisp and clear. This technology allows for maximum intensity projection, sagittal, and axial reconstructions and can display tumors, calcifications, and even blood vessels feeding the tumor.
These high-resolution images offer a real 3D view, allowing radiologists to examine any angle, which Dr. Wasser believes improves diagnostic accuracy and reduces potential oversight.
Which Future Developments do You See in the Clinical Integration of BreastCT?
Looking ahead, biopsy capabilities in breast CT should be incorporated to create a complete diagnostic platform. A biopsy option is essential, and the ability to perform it within the same breast CT session would streamline diagnosis and treatment planning. Breast CT images can also be reconstructed to resemble mammography views, enabling radiologists to work with familiar perspectives and enhancing comparability.

Dr Martin Wasser
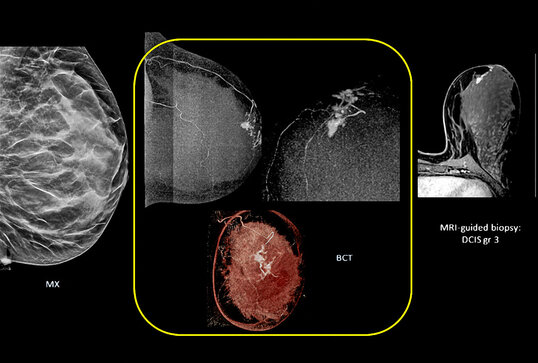
"Breast CT combines the strengths of mammography and tomosynthesis: it offers 3D imaging similar to MRI, provides high-resolution images that clearly show the morphology of the tumour and can show calcifications, which are important indicators of DCIS."
Breast-CT
This is the image of breast-CT of DCIS on breast CT (middle, in the yellow box) on sagittal, axial and frontal projection as compared to mammography (mx, left) and mri (right). BCT shows a feeding vessel to the tumor.
We will be happy to provide you with additional information on breast CT. Get in touch with us!

Online requests
You can use our contact form to send us your questions about the nu:view breast CT scanner at any time. We look forward to your inquiry.
Contact form
